A Husband and Father’s Second Chance
In 2020, a devoted husband and father underwent a successful coronary artery bypass operation, but his cardiologist and cardiac surgeons were monitoring his condition closely. He had suffered a prior stroke and was also diagnosed with peripheral vascular disease (compromised blood vessels outside the heart and brain). With the support of his family, he was carefully managing his own heart health every day.
Late one night in November, on the Sunday after Thanksgiving, he experienced the most crushing pain he had ever endured — extreme chest pressure with pain radiating to the back.
He knew something was wrong and called 911. Unfortunately, time was not on his side, as his vascular condition had taken an unexpected and dangerous turn.
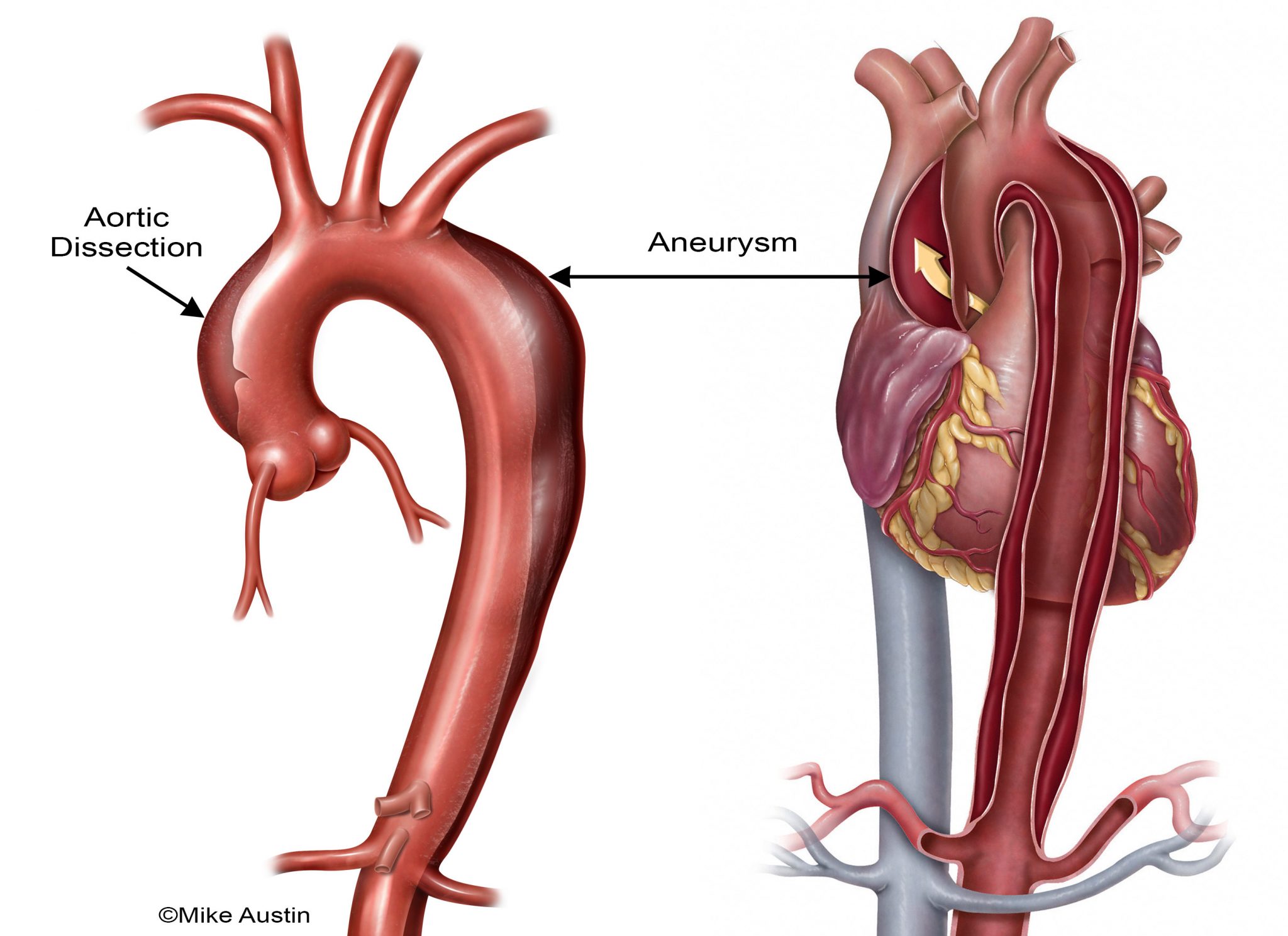
The aorta, which is the largest blood vessel in the human body, stems from the top of the heart and is shaped like a horseshoe, bending backward and downwards. This massive vessel supplies blood to the entire body. The curved section, referred to as the aortic arch, has several branches that supply blood to the arms and head.
When the walls of the aorta bulge and widen beyond their normal size, the condition is referred to as an aneurysm. If the aneurysm worsens it can tear, resulting in aortic dissection. Aortic dissection is dangerous because it can lead to rupture; since the aorta is the largest blood vessel in the body, rupture can cause excessive internal bleeding and death.
“When I heard my dad say he felt extreme chest pressure with pain radiating to the back, I strongly suspected it was an aortic dissection. This is a classic medical school board exam question,” said his son, Dr. Amit Patel.
Risk factors for aortic aneurysm include hardening of the arteries (atherosclerosis), genetic conditions such as Marfan Syndrome, and other conditions that weaken the tissues that form the blood vessel wall. High blood pressure can lead to both aortic aneurysm and aortic dissection, and trauma can cause aortic tears and rupture.
Aneurysms of the aorta may cause few or no symptoms. In fact, often, aortic aneurysms are found incidentally when a patient undergoes medical imaging for a completely unrelated health condition.
But when symptoms do arise, they need to be taken seriously. These symptoms include chest or back pain between the shoulder blades, shortness of breath, unusual fatigue, abdominal and lower back pain. Patients with any of these symptoms should seek medical help immediately.
An endovascular approach or an open surgical procedure can be used to stabilize or replace an aneurysm. In the endovascular procedure, a stent is inserted through a catheter and deployed in the weak area of the vessel. This minimally invasive treatment avoids the larger incisions required for an open surgical approach. Sometimes, though, the area where the aneurysm is located is not amenable to currently approved endovascular devices, and open surgery is needed. Thus, a multidisciplinary team approach and discussion with the patient is the best way to determine the optimum approach for each patient. Many factors go into these decisions, which are always based on the best available medical evidence that applies to the individual patient’s particular circumstances.
Repairing an aneurysm of the proximal aorta (the part of the aorta that is closest to the heart) requires a complex surgical procedure that involves stopping the heart. During this operation, a patient’s blood is circulated through the body by a heart-lung bypass machine.
Once the heart is still, surgeons replace the diseased portion of the aorta with synthetic material. If the aortic valve—the gateway from the heart to the aorta—is leaking, then the valve needs to be replaced, as well.
Call 911
On November 28, this is exactly what Mr. Patel underwent.
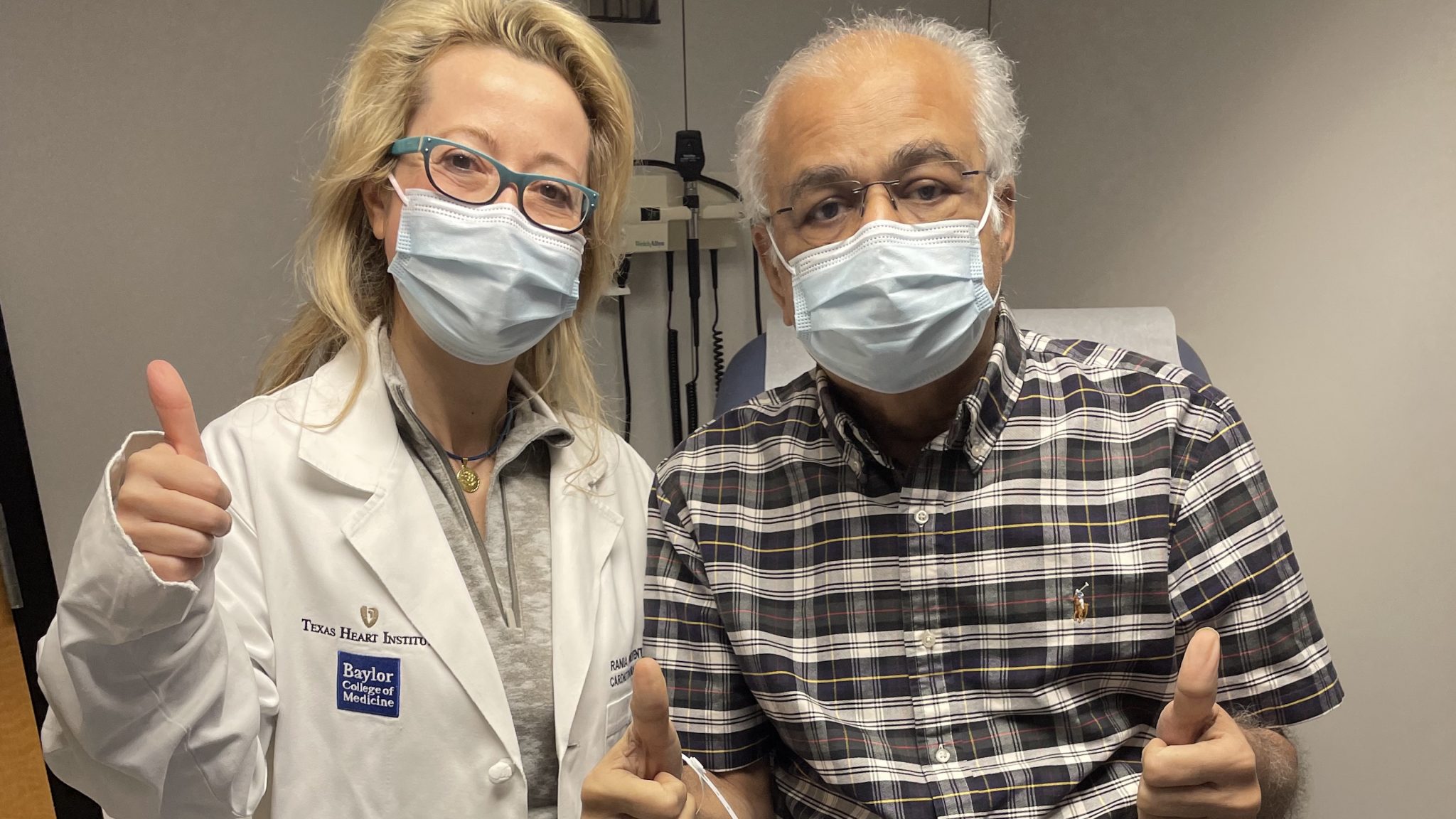
The ambulance took him to the emergency room at Baylor St. Luke’s Medical Center, and Dr. Ourania Preventza, a cardiovascular surgeon associate of the THI Professional Staff and professor of Surgery at Baylor College of Medicine, admitted him immediately. He needed surgery as soon as possible to save his life because his entire aorta was dissecting and his aortic valve was no longer functioning properly.
The unbearable chest pain and shortness of breath that Mr. Patel felt that night saved his life. His family’s suspicions were right, and his surgeons uncovered what is called an acute Type I aortic dissection with severe aortic insufficiency.
Mr. Patel needed an operation to replace his aortic valve with a prosthetic one and to replace his ruptured ascending aorta and his proximal aortic arch with a synthetic graft made of Dacron. He also needed a stent to stabilize the proximal descending thoracic aorta.
This procedure was made more challenging by the prior coronary artery bypass operation Mr. Patel had undergone for severe coronary artery disease. In that procedure, a surgical robot was used to bypass his internal mammary artery (LIMA) to his left anterior descending coronary artery; this bypass graft was still open and unobstructed (“patent”) at the time of the aortic procedure. Such grafts are lifesaving but can make subsequent aortic operations more difficult.
After Mr. Patel’s arrival to the ER late Sunday night, the complex operation started in the early hours of Monday morning and took several hours to complete.
“He had acute Type I aortic dissection with severe aortic insufficiency, which caused the aortic valve to leak,” said Dr. Preventza. “The operation he underwent is a high-risk procedure, especially for someone who has a patent LIMA-to-LAD graft from a previous coronary artery bypass operation due to extra scarring.”
The surgery was a success, and Mr. Patel is recovering well and gaining strength every day.
Mr. Patel required a prolonged recovery in the hospital, which is much more common after emergency aortic surgery than after elective aortic procedures. Ensuring that such patients have the best outcome takes a multidisciplinary approach that includes several different medical professionals.

“Whether we are resolving a question about medications or coordinating care with another clinician, we make sure to offer support not only to the patients but also to their families,” said Laura Ogbechie, MSN, FNP, a Nurse Practitioner working with the surgical team. “I believe it gives them relief when they know someone is only a phone call away. It was such a delight to see him in the clinic for a postop visit and discuss his progress. I look forward to future visits and hearing updates about his recovery.”
“At the end of the day, you see patients like Mr. Patel and realize that virtually anything is possible in medicine, and it is so rewarding,” said Dr. Preventza. “You get to save a life and give someone a second chance to spend time with family and kids. When I saw him last week for his check-up, he really made my day. It reinforces why I do what I do every day in the operating room. As a physician and health care provider, I always try to be respectful and compassionate with patients and their families. That is the only way to provide the best outcome and experience for them.”
Dr. Preventza Aneurysm Repair Lecture

.svg)


