Valve-in-Valve Aortic Repair: The Art of the Possible
Just like a person’s own aortic valve, bioprosthetic replacement valves can become calcified or stenotic (narrowed) over time, which can prevent the valve from opening completely with each heartbeat.
Rather than subjecting a patient to another open-chest surgery to replace or repair a dysfunctional bioprosthetic valve, surgeons may be able to place a new transcatheter valve into the existing valve by accessing the heart through a blood vessel, as described in a recent case report from cardiothoracic physicians at The Texas Heart Institute and Baylor College of Medicine in Houston, Texas.
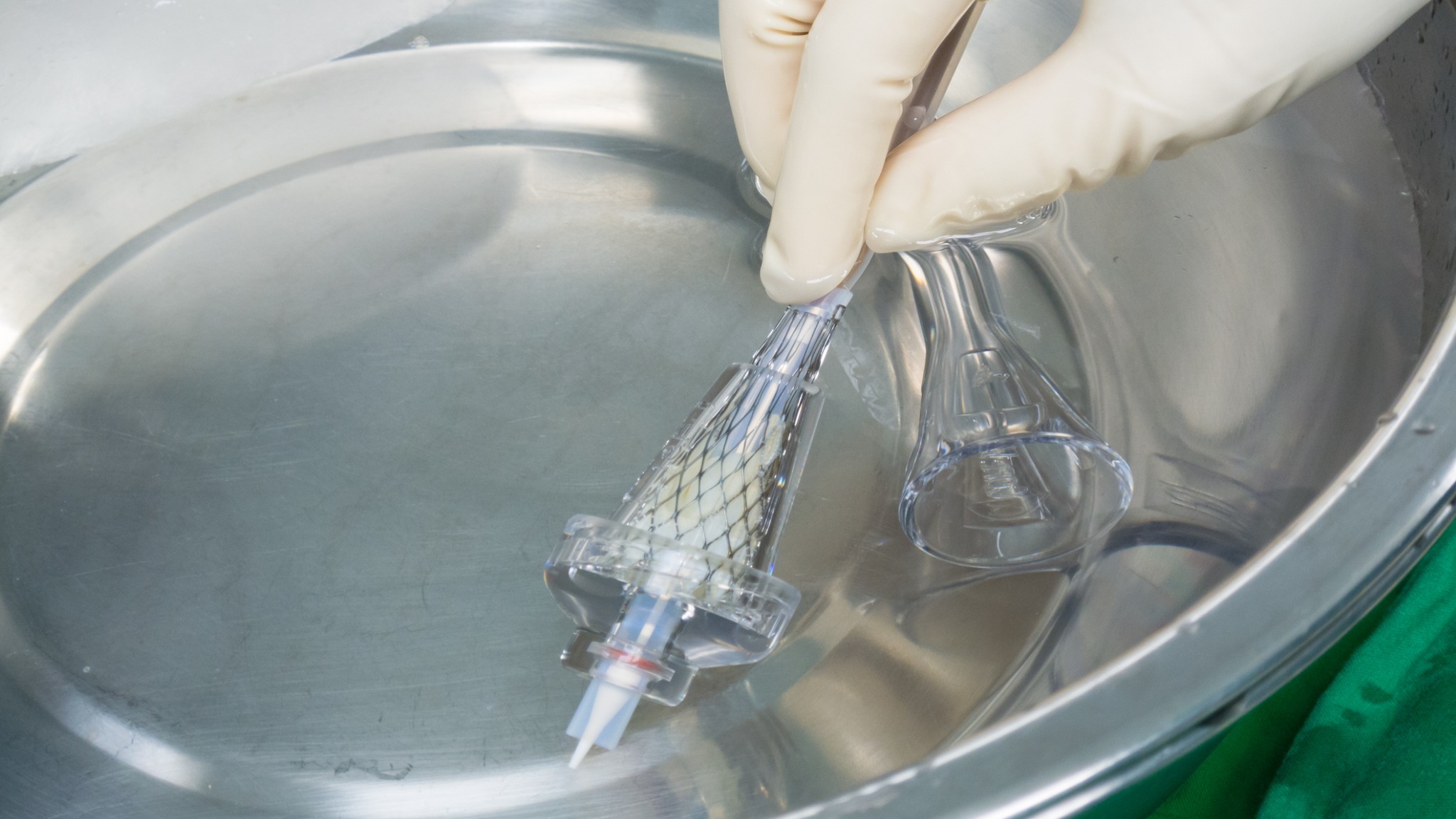
This so-called “valve-in-valve” approach was used in a 61-year-old patient who 5 years previously had undergone aortic valve replacement with a 25-mm Edwards INTUITY Elite bioprosthetic valve; this valve is made of bovine pericardial tissue and a metal stent framework that includes a stainless steel “skirt” for support.
As a rapid deployment valve, the INTUITY Elite requires far fewer sutures during surgery than traditional aortic valves. It is expanded with a balloon to seal and secure the valve’s skirt after the patient’s own aortic valve is removed.
At this patient’s annual checkup, calcium deposits were found on the INTUITY valve’s leaflets. These deposits can cause structural deterioration and severe narrowing of the valve opening, which impedes blood flow through the valve.
Case discussion by a multidisciplinary care team led to the decision to use a femoral artery approach to deploy a 29-mm Medtronic Evolut PRO+ self-expanding transcatheter valve within the patient’s existing INTUITY valve.
The new valve was positioned flush with the bottom of the INTUITY valve’s skirt—intentionally lower than generally recommended—to avoid blocking the coronary arteries, which supply oxygenated blood to the heart itself. Mild leakage around the valve after it was deployed was corrected with additional careful balloon expansion. The patient recovered well and was discharged two days later.
Rapid-deployment bioprosthetic valves like this patient’s INTUITY device have gained widespread use for valve repair. Valve-in-valve placement of a transcatheter valve within one of these existing bioprosthetic valves avoids the injury and complications associated with redo sternotomy and is therefore of great interest to both patients and surgeons. Both balloon-expandable and self-expanding transcatheter valves can be used for valve-in-valve placement, with similar survival outcomes.
Caveats inherent with valve-in-valve procedures include a considerable frequency (up to 25%) of persistently strained pressure across the valve, the risk of getting a valve that is slightly too big or too small for the patient’s body size, the need for a pacemaker, and overexpansion of the INTUITY valve skirt during deployment of the new valve, which can rupture the aorta.
Said senior author Joseph S. Coselli, MD, cardiothoracic surgeon at Baylor College of Medicine and the Texas Heart Institute, “In this particular case, we showed that a self-expanding Evolut transcatheter valve can be successfully implanted into a degenerated, stenotic INTUITY valve. To our knowledge, this specific approach had not been described in the literature before we published our case report. By positioning the Evolut valve a bit lower than the manufacturer suggests, we were able to maintain reasonable space for future coronary artery access, if needed, yet still achieve good hemodynamic outcomes and reduce strain across the valve.”
Read Report
Farmer DM, Diez JG, Orozco-Sevilla V, Coselli JS. Use of a self-expanding transcatheter valve for a degenerated INTUITY valve. J Card Surg. 2022 Oct;37(10):3413-3416. doi: 10.1111/jocs.16746
News Story by Jeanie F. Woodruff, BS, ELS

.svg)


