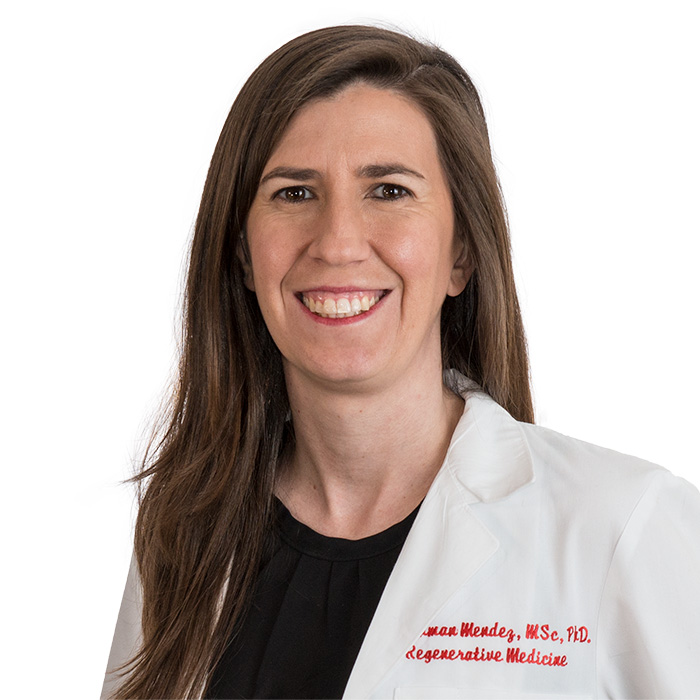
Dr. Camila Hochman-Mendez is the Texas Heart Institute’s Assistant Director of Regenerative Medicine Research and Director of the Biorepository and Cell Profiling Lab. Dr. Hochman-Mendez’s research centers on the role of extracellular matrix proteins on cardiac stem cell differentiation, tissue repair, and regeneration.
Show full bioTexas Heart Institute Positions
- Assistant Investigator; Director, THI Biorepository and Cell Profiling Lab
- Assistant Investigator; Assistant Director, Regenerative Medicine Research
Honors, Awards and Memberships
Publications
Recent News
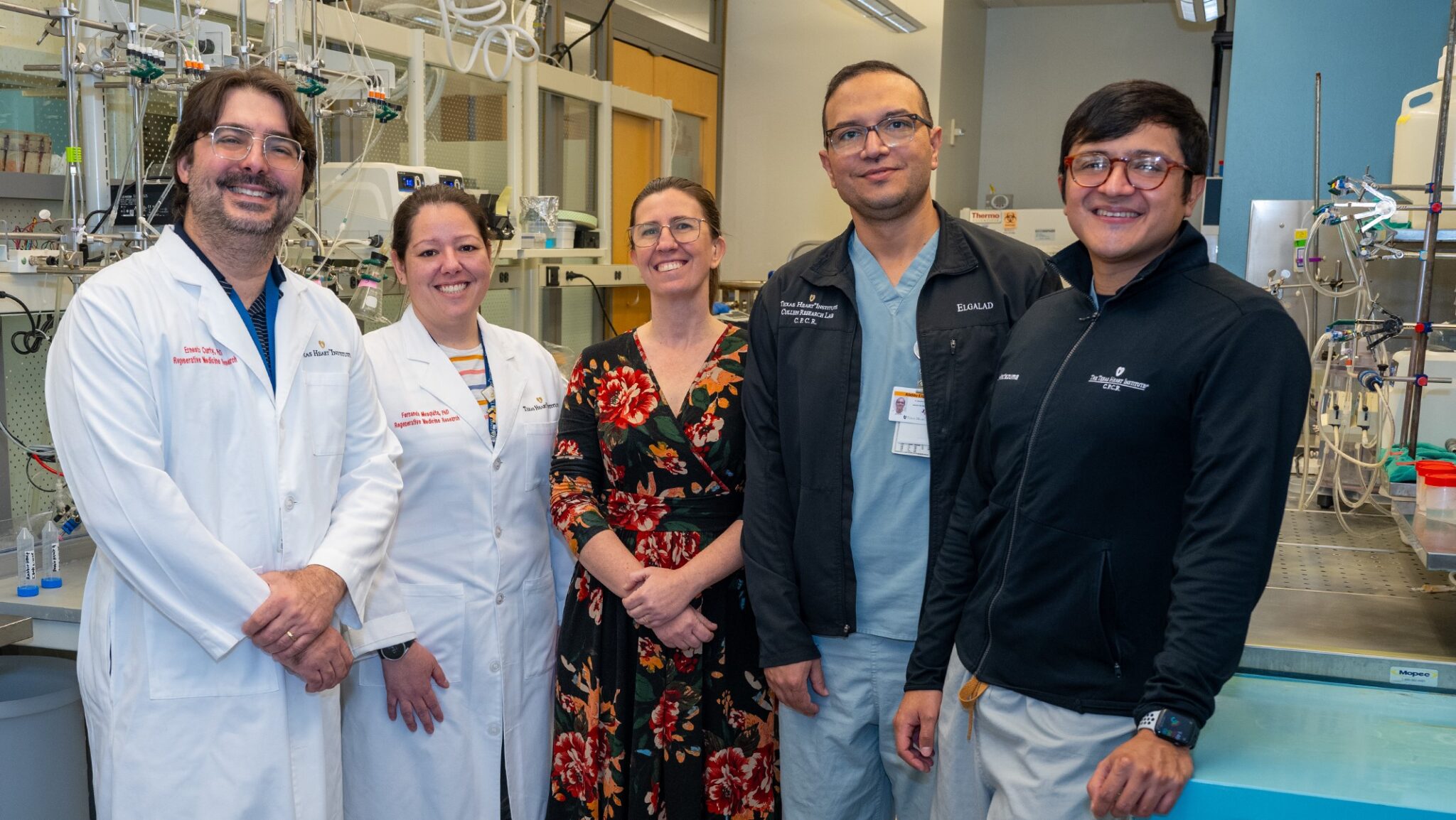
Researchers at The Texas Heart Institute Pioneer Light-Responsive and Wireless Cardiac Stimulation Technologies
Researchers at The Texas Heart Institute (THI)—Camila Hochman-Mendez, Fernanda C. Paccola Mesquita, Ernesto Curty da Costa, Angel Moctezuma-Ramirez, and Abdelmotagaly...
Celebrating Women in Science at The Texas Heart Institute
As the world celebrates the International Day of Women and Girls in Science, a day dedicated to recognizing the invaluable...
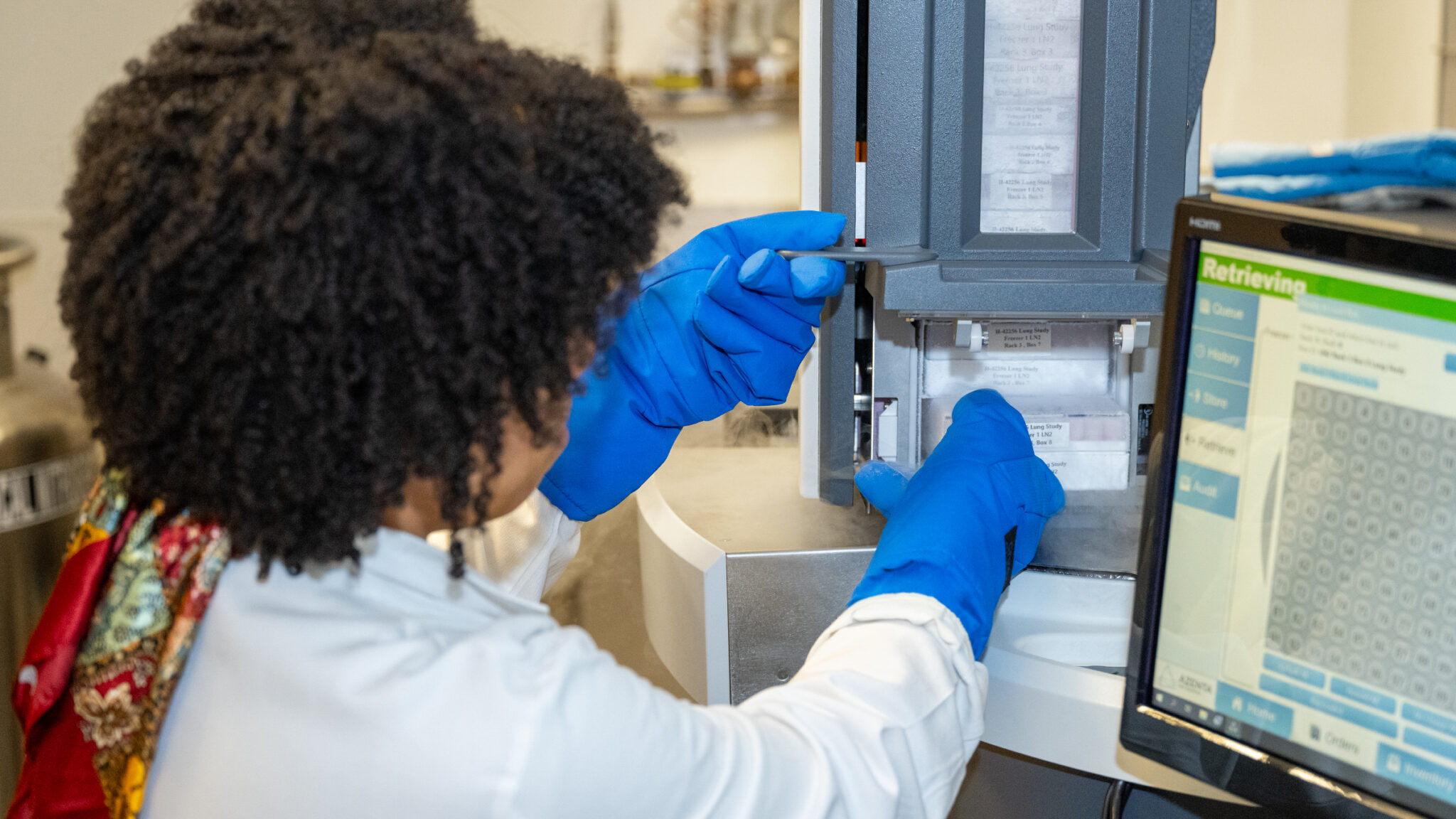
The Texas Heart Institute Biorepository Demonstrates Excellence in Sample Quality with New Publication
A Study Validates THI’s Biorepository as a Global Leader in Long-Term Sample Preservation and Quality Assurance The Texas Heart Institute...

.svg)


