45 Years of Innovation
With over 45 years of innovation under its belt, the Center for Preclinical Surgical and Interventional Research and world-renowned Cullen Cardiovascular Research Laboratory is committed to harnessing the expertise of its talented team. Through its in-house work and collaborations with other institutions, it has become one of the most treasured resources in the Texas Medical Center.
Forging New Paths in Research
The Texas Heart Institute’s Center for Preclinical Research (CPCR) is a leading research department that collaborates with teams around the world in the design, development, and testing of a range of innovative devices. Founded in 1972, the CPCR reflects the high standards of excellence established by Dr. Denton Cooley and Dr. O.H. Frazier, over the past five decades. Today, the CPCR has the resources to design and execute translational studies that will lead to the next major advancement in cardiovascular research. The CPCR accommodates the in vivo research of interventional cardiologists, cardiovascular surgeons, cell biologists, and regenerative medicine specialists at THI in an effort to treat heart disease more effectively and provides the infrastructure for important research efforts of outside investigators and study sponsors.

The Center for Preclinical Surgical and Interventional Research (CPCR) supports Texas Heart Institute’s surgical and interventional cardiology in many ways, including medical device development and testing, pharmacological testing, efficacy testing of various regenerative treatments, and developing physician training programs for FDA-approved medical devices.
To perform a wide array of experiments, the Center encompasses a 20,000 square-foot facility with modern operating suites, a 24/7 ICU, chronic invasive and noninvasive monitoring units, necropsy and histopathology lab support, and in vitro testing capabilities.
The facility is USDA licensed, AAALAC accredited since 1994, and GLP compliant. With constant innovations to research capabilities, the CPCR team will soon have a clinical-grade cardiac catheterization laboratory, which will significantly advance research and innovation at THI through the new Phillips Azurion 7 Series technology, whose 3D imaging tool can provide real-time HD images showing complex cardiac anatomy and electrophysiology navigation mapping, and the Xper CT, which will allow head-to-toe 16 bit CT imaging capability and access to the patient from all sides.
Many surgical projects are currently underway: mechanical support device testing such as total artificial heart and ventricular assisted devices, tissue-engineered vascular grafts, organ procurement with ex vivo organ perfusion and experimental heart or lung transplantation, and more. As far as interventional projects go, the CPCR has multiple efforts in this arena as well, including catheter delivery of innovative gene and stem cell therapy products, innovative electrophysiology studies, minimally invasive heart pumps, and prototype balloons and catheters. The lab also extends the scope of work to support other research areas like urology with a total bioartificial kidney study, and abdominal surgery, and many other projects throughout the Texas Medical Center.
Pumped Up About Cardiovascular Research
Since 1972, O.H. Frazier, MD has been studying surgical devices. For years, his research focused on pulsitile blood flow. However, in the 80s, when postal pumps were shown to lack endurance, lasting 2 years at best, Dr. Frazier shifted his research approach to non-pulsitile blood flow. At this critical junction, Dr. Frazier went against prevailing scientific evidence and realized that continuous-flow pumps were a necessity. Out of this necessity sprung an invention: a continuous-flow pump that has been used in more than 60,000 patients around the world, thanks to the innovation of Dr. Frazier.
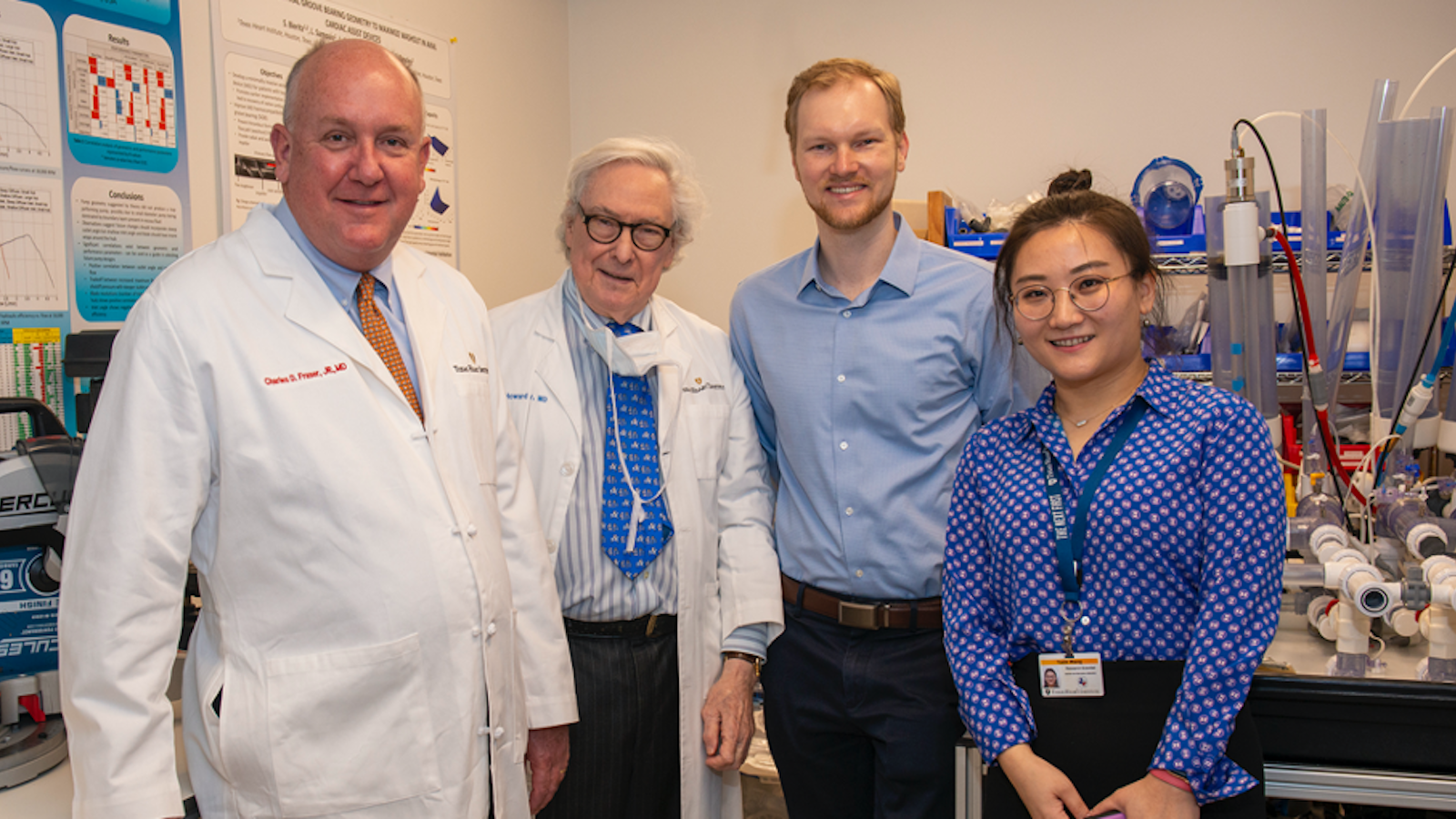
At the Cullen Cardiovascular Research Laboratory at THI, Dr. Frazier currently focuses his research on another necessity: a small pump that is placed in the left atrium to decompress the heart and take the burden off the ventricles patients with early-stage heart failure. Dr. Frazier has been working in collaboration with Yaxin Wang, PhD to address some of the real engineering problems that must be overcome for a long-term device to be successful.
Engineering Challenges
To identify the optimal pump that reaches the design goal of 2 liters per minute and 90 millimeters Mercury, Dr. Wang ran 32 different pump designs through a battery of tests, starting with hydraulic testing and progressing to preclinical testing once a successful design was identified. Once the selection of pump candidates was narrowed down, a collaboration was started with Katherine Fraser of the University of Bath to reduce the rate of hemolysis (ie, breakdown of red blood cells). In another strategy, a hydrodynamic bearing test rig is utilized to test a secondary rotor with a different bearing in the pump. A mock circulatory loop has also been created to simulate the human cardiovascular system and test pump capabilities.
Strong engineering support is driving the production of these small pumps to assist in long-term solutions that would be key to saving many children’s lives, as such equipment is not currently available for children younger than 9 years old. Dr. Frazier and his team are committed to the creation of this pump and solving more of the challenges of heart failure.

.svg)



