The Next First
"We are pioneering some of the most groundbreaking cardiac arrhythmias research and management today in collaboration with institutions across the US. With a history of firsts in man devices, the next first in cardiac arrhythmia treatments is already happening at the Texas Heart Institute." Mehdi Razavi, MD
Clinically Speaking: Answering the Unanswerable
From a clinical perspective, the EPCRI Lab seeks to find solutions to unanswered questions in the field by performing data studies in which clinical data are entered and reviewed. Then, the statistical analysis of data and the delivery of information to physicians in a more understandable way ultimately improve patient management. Several different types of clinical studies are conducted in the EPCRI Lab, including case reports, case series, meta-analyses, and randomized controlled trials. Research currently in progress involves new catheters, as well as novel methods for ablation and mapping. Another interesting project builds upon a previous study by the Lab on the role of influenza in cardiac shock. This study is receiving a great deal of attention for its relevance to COVID-19.
The EPCRI Lab is a turn-key lab that can perform all of the steps of clinical studies from A to Z and is eager to collaborate with others to advance cardiac care.
A primary goal at THI is increasing physician knowledge and using state-of-the-art devices and strategies to create technologies and therapies that advance patient care. The Electrophysiology Clinical Research and Innovation (EPCRI) Lab leads the charge in this area. With Director Mehdi Razavi, MD, at the helm, the Lab’s mission is to develop, conceptualize, and validate new technologies in cardiac electrophysiology and cardiology in general.
How does this process work? Once a concept is borne, iterative testing begins. If the technology is successful, clinical trials are performed. Many of the technologies developed at THI turn into startup companies or licensing deals to ensure that patients reap the benefits. By generating innovative ideas, Dr. Razavi and his team have ultimately improved patient outcomes.
Ongoing Projects
The EPCRI Lab has several ongoing projects at different stages—all of which are potentially life-changing for patients.
One in 5 patients is affected by internal bleeding. The startup company Saranas (Houston, TX) that was founded on technology designed and tested at THI has developed a modified sheath with electrodes on it that sense bioimpedance in real time and determine the rate of bleeding in a patient during a procedure. This can aid physicians in mitigating blood loss and determining postoperative care procedures.
“The ‘Triple Crown’ of treating both the most common and the most lethal cardiac arrhythmias is external powering, wireless pacing and—far and away most importantly—cardiac defibrillation that is not only painless but is actually imperceptible to the patient. Our technology brings into sharp focus the remarkable possibility of achieving this goal.”
–Mehdi Razavi, MD, Director, Center for Electrophysiology Clinical Research and Innovations
Another large project in the works is an NIH-funded, leadless pacemaker that could prevent several common complications. Instead of requiring a battery, this device would be charged wirelessly like a smartphone. Miniature nodes would be able to pace and sense in multiple locations, which may lead to new treatment strategies that utilize multisite pacing.

A novel material called carbon nanotube fiber is being developed in the EPCRI Lab by using funding from the AHA. These fibers can be directly deployed onto the heart to bridge areas of scarred myocardium and reduce future arrhythmias.
Rewiring Hearts With Nanotubes Soft fibers bridge gap to restore healthy beat. (n.d.). Rice Magazine Winter 2020, 25. Graphic by Daisy Chung
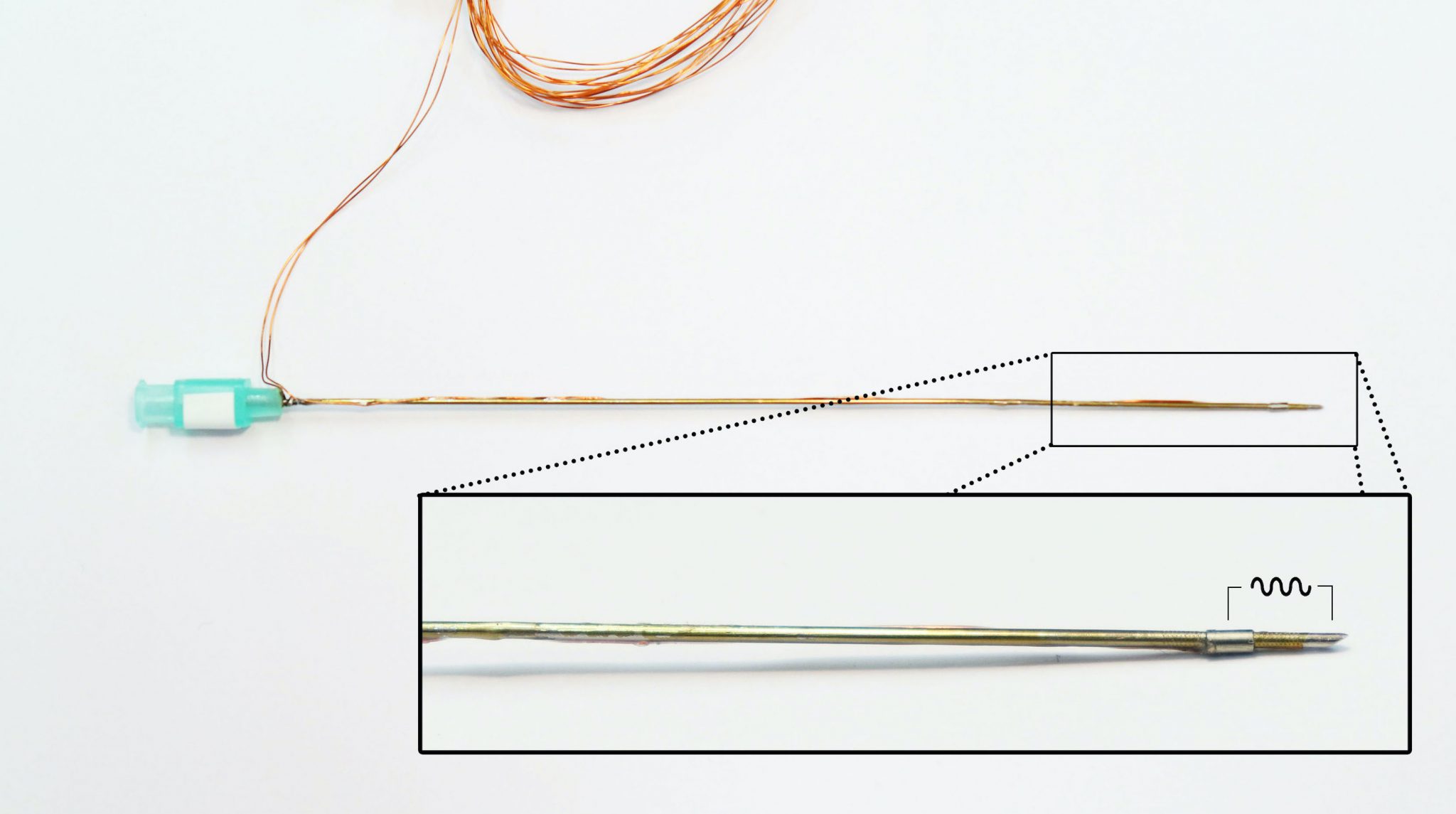
Some projects do not involve new therapies but have the potential to provide physicians with better diagnostic and treatment capabilities. An example is the newly modified microfunction needle, which is a 21-gauge needle that has an electrode on it. The needle’s tip can measure bioimpedance to improve pericardial and vascular access and better differentiate tissues to avoid surgical complications.
In collaboration with the University of Texas (UT) at Austin, THI is expanding pacing capabilities by using conductive hydrogels that can be deployed into any vein of choice by connecting them to a pacemaker lead. This extension of the lead can be utilized in new therapies that are currently not possible. The NIH grant proposal for this project was rated in the top 2% and is expected to be funded this spring.
A collaboration currently in progress with Rice is the utilization of machine learning for a multitude of functions, including the detection and classification of disease. By providing the electrophysiologist with specific data obtained in a minimally invasive manner, this technology will certainly lead to improved clinical outcomes.
Lab Workflow – How Research Gets Done
Projects are first evaluated against the Lab’s mission to determine feasibility. The Lab has 2 development pathways with distinct goals: the creation of new technologies or therapies and the advancement of knowledge in the field.
In the first pathway, brainstorming is the first step of creating new technologies after a clinical need is identified. Then, a decision is made as to whether a process change needs to occur or a new device needs to be designed. The other pathway of the Lab expands knowledge by testing known technologies and possibly changing operating protocols to advance techniques in the electrophysiology world. The two pathways both culminate with prototyping and engineering of solutions, intellectual property generation, and, lastly, implementation testing. To aid in this process, the lab has the capability of designing electronics and devices by using 3D printing.
Collaboration is always key at THI, and the EPCRI Lab is no exception. They have strong, productive working relationships with Rice, UCLA, UT Austin, Baylor College of Medicine, UH, and Texas A&M.

.svg)



