
Honors, Awards and Memberships
Publications
Recent News
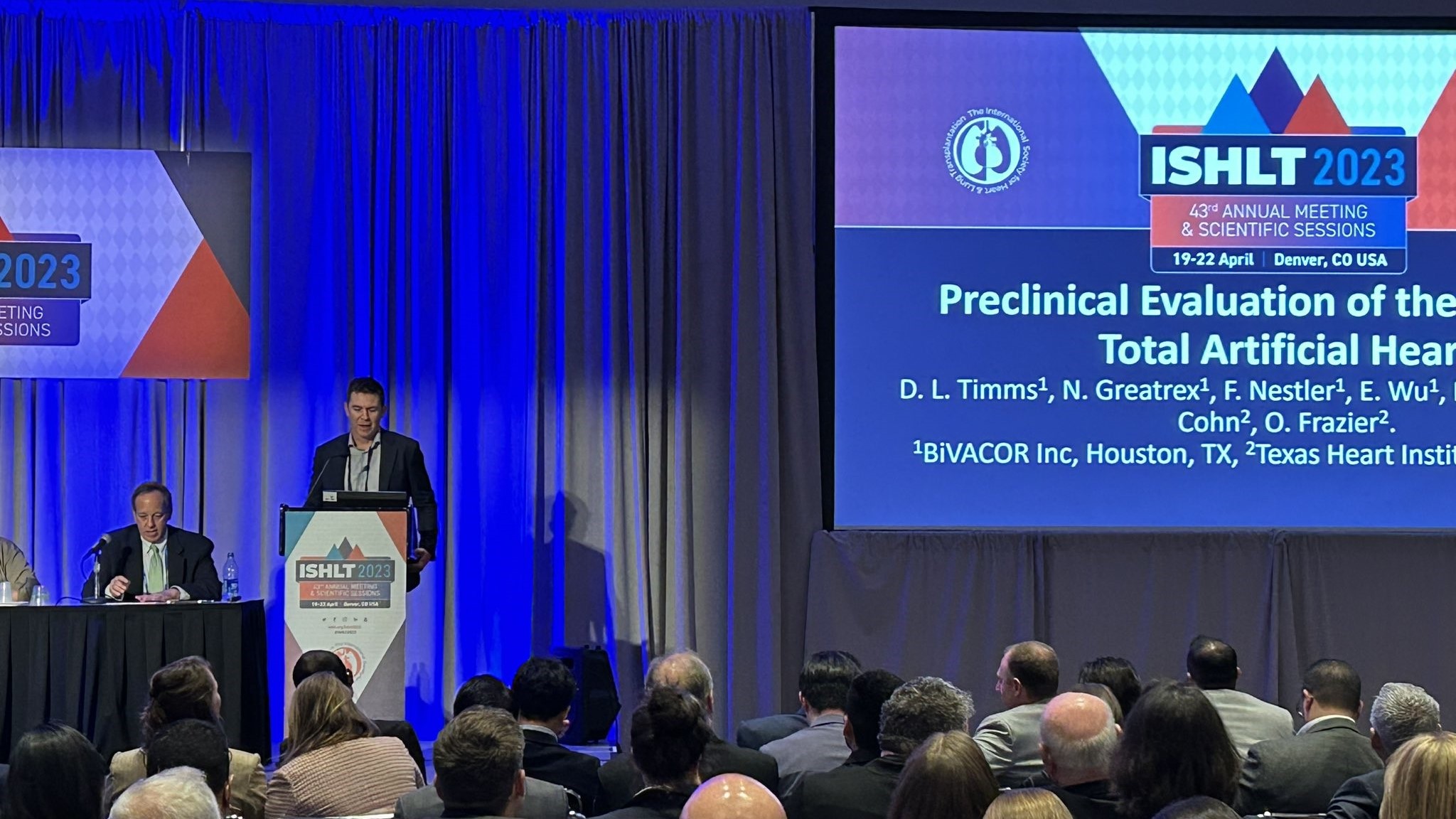
The Texas Heart Institute Makes a Strong Showing at ISHLT 2023
Daniel Timms, PhD, founder and chief technical officer of BiVACOR, Inc., described the benchtop testing and preclinical studies performed with...

Sharing Our Latest Research With the World
Our Professional Staff members have demonstrated a commitment to advancing cardiovascular science. This can be seen in their research output....

Meet Dr. Clauden Louis AATS 2022 Denton A. Cooley Fellow
“This has been an amazing experience. To know that I’m not only carrying the name of one of the giants...

.svg)


