
James J. Livesay, M.D. is an accomplished surgeon with extensive experience in cardiovascular, thoracic, and general procedures. An Associate Surgeon at the Texas Heart Institute (THI), Houston, Texas, since 1981, Dr. Livesay is also an Associate Surgeon at Baylor St. Luke’s Medical Center, Houston, Texas, and is on the Consulting Staff, Cardiovascular Service, Texas Children’s Hospital, Houston, from that time. He was a member of the Active Staff, General Surgery and Thoracic and Cardiac Surgery, Gulf Coast Hospital, Wharton, Texas, from 1989 to 2013, and held a Courtesy Staff position in General Surgery and Thoracic and Cardiac Surgery at Hermann Hospital, Houston, Texas from 1982 to 1998. He is Clinical Associate Professor of Surgery, University of Texas Medical School, Houston, Texas.
Show full bioJames J. Livesay, M.D. received the Doctor of Medicine degree from Baylor College of Medicine, Houston Texas, which he attended 1969-1973 after graduating (B.S. Cum Laude) from Washington and Lee University, Lexington, Virginia, in 1969. Dr. Livesay did his internship and surgery residency training at University of California Los Angeles Center for Health Sciences 1973-1975. He then did a Research Fellowship in Cardiac Physiology at the University of California Los Angeles, Division of Cardiovascular Surgery from 1975 to 1976, becoming Resident and Chief Resident in Surgery, University of California Los Angeles Center for Health Sciences, a position he held from 1976 to 1979. He also completed a Residency training in Thoracic and Cardiovascular Surgery at the Texas Heart Institute, and M.D. Anderson Hospital and Tumor Institute, Houston, Texas, from 1979 to 1981.
Texas Heart Institute Positions
- Surgery, The Texas Heart Institute Center for Cardiovascular Care
- Teaching Staff, Thoracic Surgery Residency
- Teaching Staff, Denton A. Cooley Fellowship
- Editorial Board, Texas Heart Institute Journal
Education
-
Undergraduate:
Washington and Lee University (Lexington, Virginia)
-
Medical School:
Baylor College of Medicine
-
Internship:
University of California Los Angeles Center for Health Sciences
-
Residency:
University of California Los Angeles Center for Health Sciences
-
Fellowships:
University of California Los Angeles Center for Health Sciences
Texas Heart Institute
M.D. Anderson Cancer Center
Academic & Clinical Affiliations
- The Texas Heart Institute Center for Cardiovascular Care
- Baylor College of Medicine
- Baylor St. Luke's Medical Center
Honors, Awards and Memberships
Publications
Recent News

THI Perfusion School Honors Asia Nguyen With Sal Guercio Memorial Scholarship
The Texas Heart Institute School of Perfusion Technology has honored student Asia Nguyen with the third annual Sal Guercio Memorial...
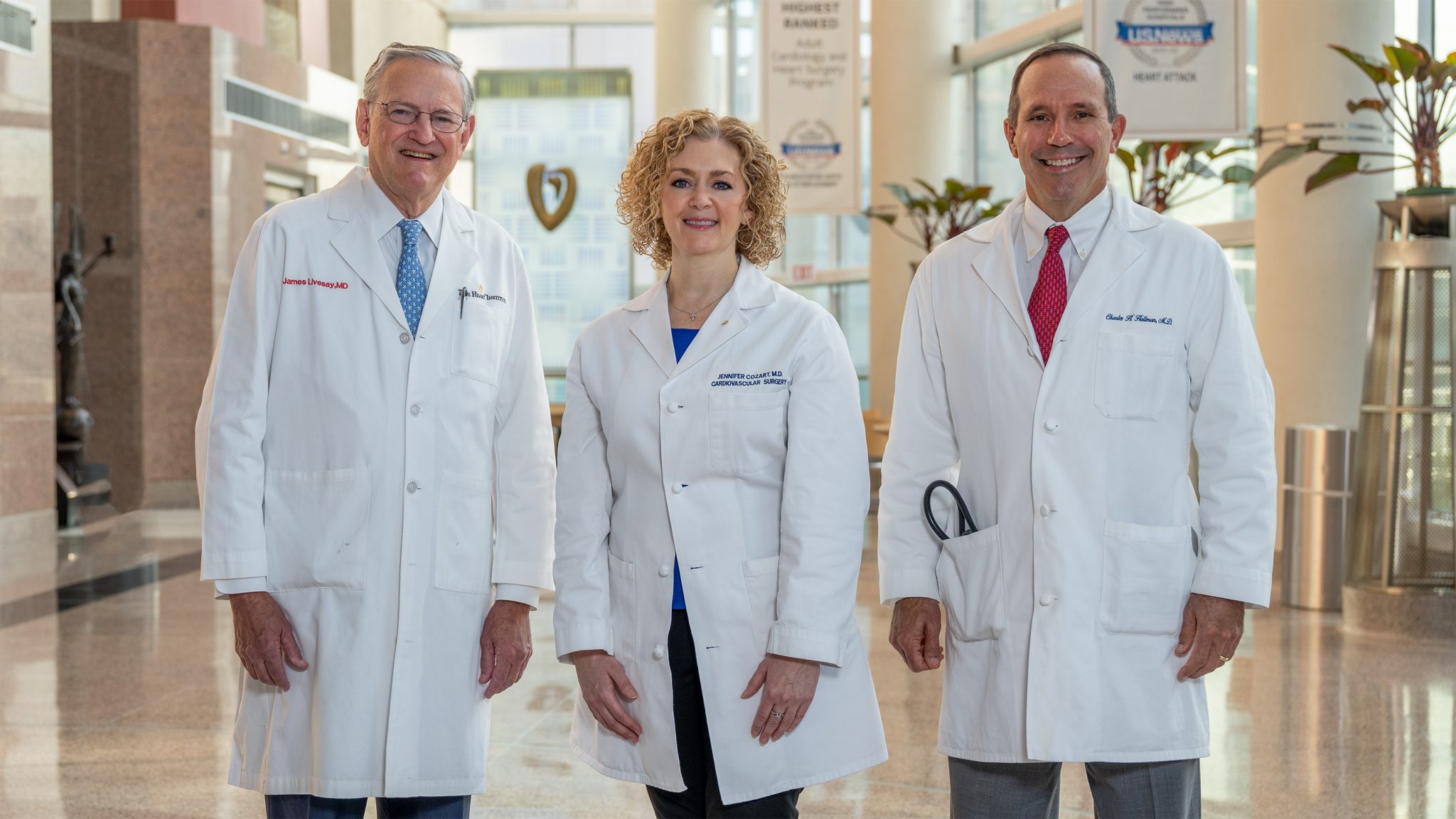
Texas Heart Institute Surgeons Recognized for Quality Care
HOUSTON, TX, February 15, 2024— Three Texas Heart Institute Center for Cardiovascular Care surgeons, Drs. James Livesay, Jennifer Cozart and...
International Interactive Symposium Welcomes Experts from Across the US and Around the Globe
HOUSTON (Oct. 23, 2023) — The International Society for Endovascular Specialists (ISEVS) celebrated its 30th anniversary with a prestigious symposium...


