
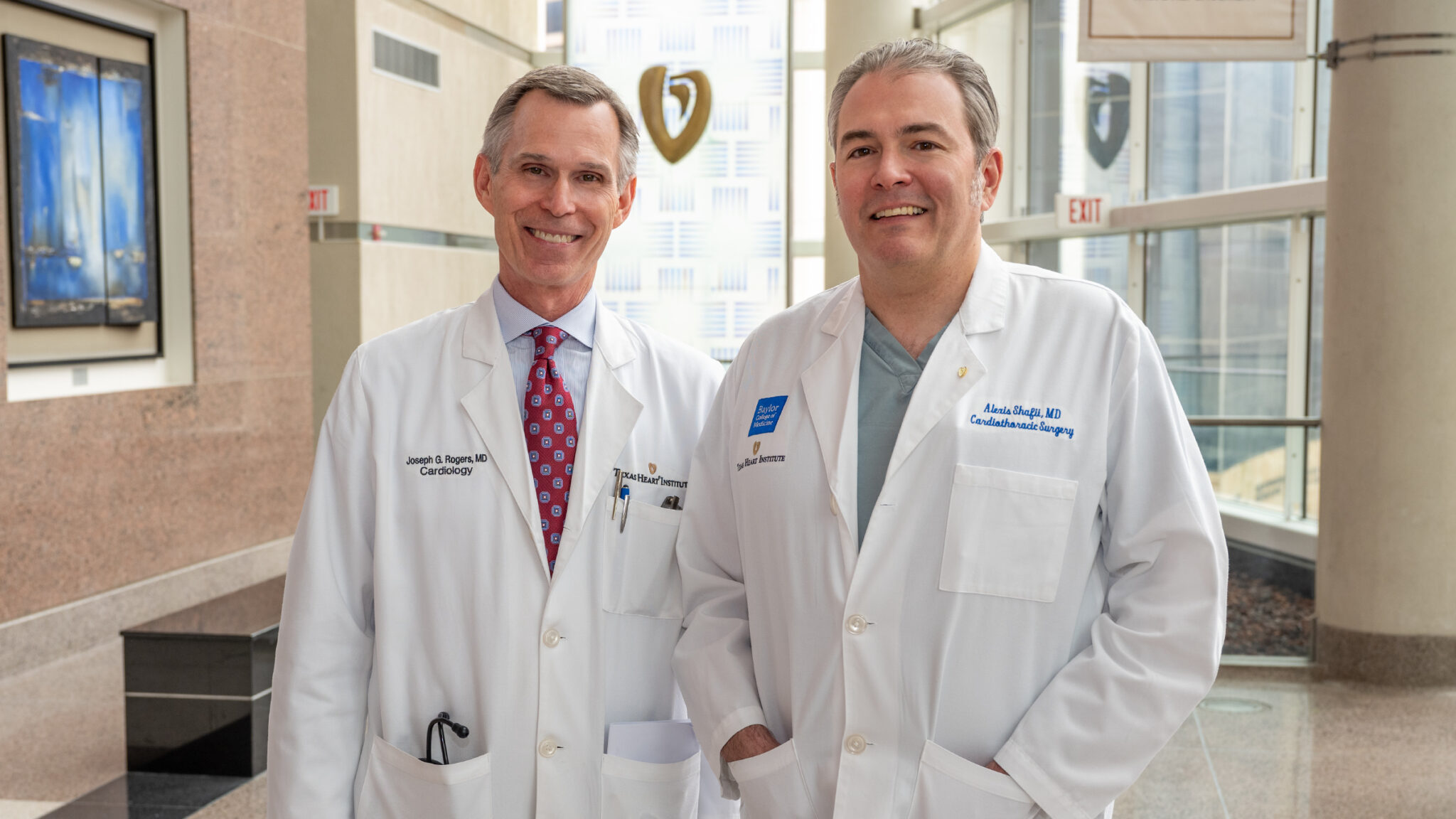
Dr. Alexis Shafii is a cardiothoracic surgeon with expertise in thoracic transplantation and adult cardiac surgery.
Show full bioHis clinical focus includes thoracic organ failure, heart and lung transplantation as well as implantation of mechanical circulatory support devices. He is the surgical director of the heart transplant program at Baylor St. Luke’s Medical Center, and previously directed transplant programs at major medical centers in Dallas and Kentucky.
Dr. Shafii also treats adult acquired cardiac diseases, including coronary artery disease, heart valve disease, and aortic pathologies. His research efforts focus on heart and lung transplantation, ventricular assist devices, and extracorporeal membrane oxygenation (ECMO).
Interests
- Heart and Lung Transplant
- Cardiac Surgery
Education
-
Undergraduate:
Boston College
-
Medical School:
University of South Florida College of Medicine
-
Residency:
University of South Florida College of Medicine
-
Fellowships:
Cleveland Clinic Foundation
Certifications
- American Board of Surgery
- American Board of Thoracic Surgery
Honors, Awards and Memberships
- Houstonia Magazine Top Doctor
- American College of Surgeons
- The International Society for Heart and Lung Transplantation
- Society of Thoracic Surgeons
- The Texas Heart Institute Academic Professional Staff
Publications
Recent News
The Texas Heart Institute Provides BiVACOR® Total Artificial Heart Patient Update
Successful first-in-human bridge to heart transplant with revolutionary valveless artificial heart Houston, Texas, July 26, 2024 – The Texas Heart...
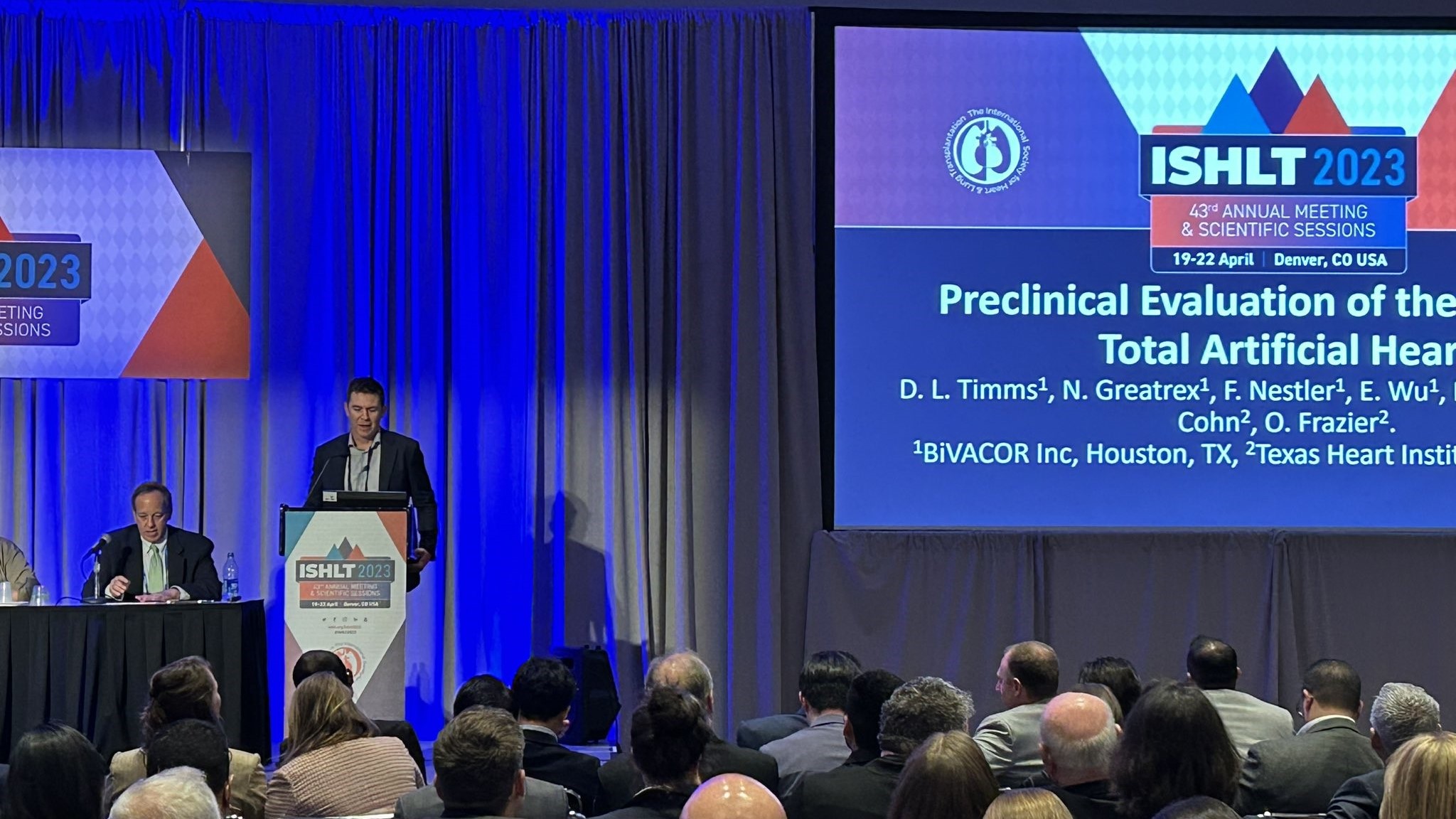
The Texas Heart Institute Makes a Strong Showing at ISHLT 2023
Daniel Timms, PhD, founder and chief technical officer of BiVACOR, Inc., described the benchtop testing and preclinical studies performed with...

Sharing Our Latest Research With the World
Our Professional Staff members have demonstrated a commitment to advancing cardiovascular science. This can be seen in their research output....

.svg)


