
Dr. Abdi Rasekh is an interventional cardiologist, electrophysiologist and member of The Texas Heart Institute (THI) Professional Staff. Since completing his cardiology and cardiac electrophysiology fellowships at THI, he has served as a member of the teaching staff for the fellowship programs and participated in several clinical research projects.
See PublicationsTexas Heart Institute Positions
- Teaching Staff, Cardiovascular Disease Fellowship
- Teaching Staff, Clinical Cardiac Electrophysiology Fellowship
- Editorial Consultant, Texas Heart Institute Journal
Interests
- Sudden cardiac death
- Atrial fibrillation
- Ablation of arrhythmias
- Device therapy for congestive heart failure
- Management of coronary artery disease
Education
-
Graduate:
Graduate Hospital of University of Pennsylvania in Philadelphia
-
Medical School:
University of Paris XIII, Bobigny School of Medicine
-
Internship:
The Graduate Hospital Department of Medicine, University of Pennsylvania
-
Residency:
The Graduate Hospital Department of Medicine, University of Pennsylvania
-
Fellowships:
Texas Heart Institute/Baylor College of Medicine (Cardiology)
Texas Heart Institute/Baylor College of Medicine (Clinical Cardiac Electrophysiology)
Academic & Clinical Affiliations
Certifications
- Board Certified, Internal Medicine, Cardiovascular Disease, Interventional Cardiology & Clinical Cardiac Electrophysiology
Honors, Awards and Memberships
- The Texas Heart Institute Academic Professional Staff
- Bronze Medical Award for Clinical Research Thesis, University of Paris XIII
- Chief Fellow, Texas Heart Institute Cardiology Disease Fellowship at St. Luke's
- Member, Heart Rhythm Society
- Fellow, American College of Cardiology
Publications
Recent News
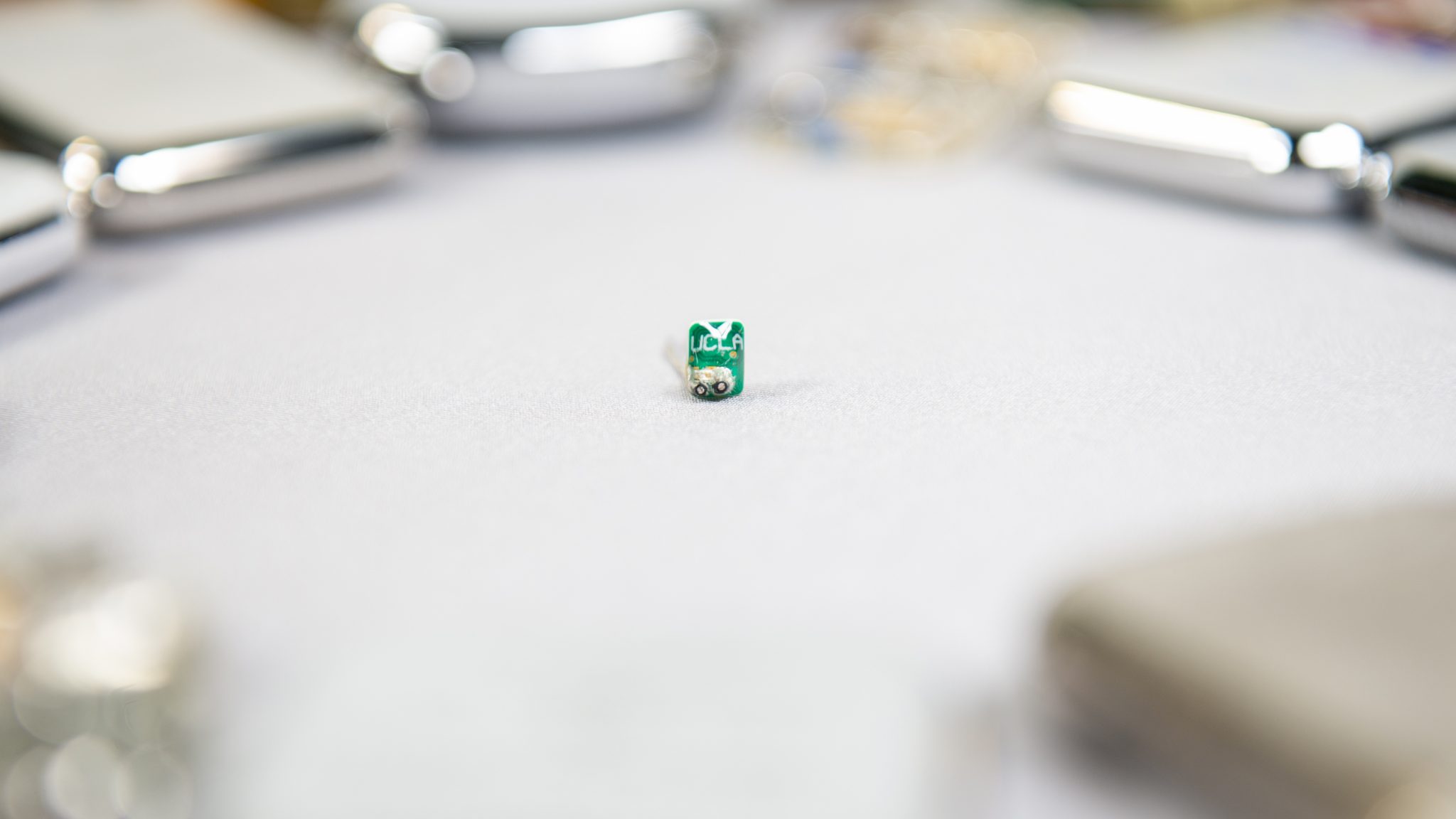
Doctors and engineers tackle two major challenges in heart care
In these challenging times, innovative ideas are needed more than ever. An article about Dr. Mehdi Razavi and the Electrophysiology Clinical...

Best Practices & State of the Art Approaches in the Treatment of Cardiac Arrhythmia
The Ali Massumi Cardiac Arrhythmia Symposium is designed to provide cardiac electrophysiologists, cardiologists, internists, fellows, cath lab technicians, family and general practitioners...

Sharing Science Globally to Advance Medicine
Texas Heart Institute has been at the forefront of cardiovascular discovery and innovation since its formation. It continues to relentlessly...


