Engineered stem cells show promise for new treatment of peripheral arterial disease
Houston, TX (June 1, 2016) – Stem cells have been shown to produce a variety of substances that promote tissue repair and help protect healthy cells exposed to hazardous conditions; thus, these cells have great potential as therapeutic agents. Researchers at the Molecular Cardiology Research Lab at the Texas Heart Institute are currently investigating the role of stem cells in tissue repair and developing cell-based therapies for patients with cardiovascular diseases. In an article recently published in Nature Communications, these researchers describe their innovative new strategy to enhance the benefits of stem cell therapy for the treatment of peripheral arterial disease (PAD).
Many cardiovascular diseases are caused by plaque build-up within the blood vessels, which can reduce blood flow and oxygen supply to the tissues (a condition known as ischemia). When this plaque build-up reduces blood flow to the limbs, the person can develop PAD. In severe cases of PAD, the affected limb can develop gangrene and may need to be amputated. In some cases, PAD can be treated with surgery, but for patients with PAD who are poor candidates for surgical treatment, an alternative treatment option is urgently needed.
One such option is prostacyclin. Prostacyclin is a drug that dilates (or widens) blood vessels and prevents the formation of blood clots inside the vessels; however, because prostacyclin has a circulating half-life of only 1-2 minutes, it must be given continuously, either intravenously or directly into the artery. This approach can potentially decrease the patient’s quality of life because the delivery system is cumbersome, and it can lead to severe complications, such as infusion-site infections.
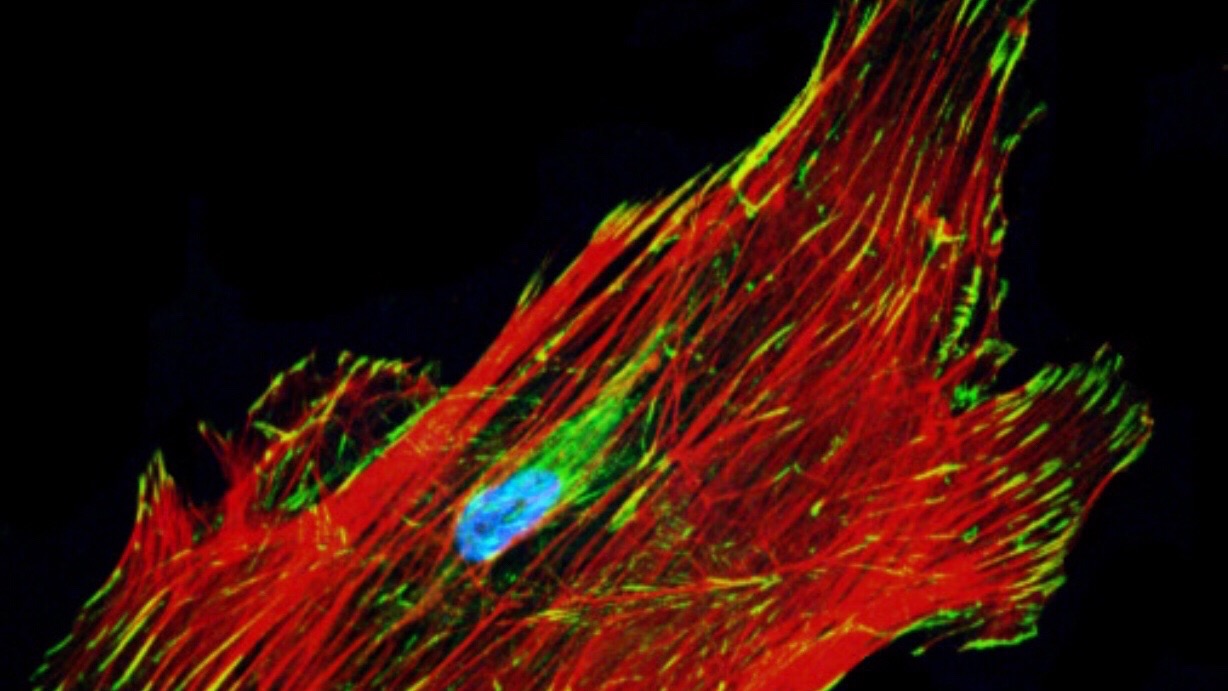
To overcome these complications, investigators at the Molecular Cardiology Research Lab have produced engineered human mesenchymal stem cells (hMSCs) that consistently secrete prostacyclin and used these cells as a vehicle to directly deliver prostacyclin to the ischemic limb, thus combining the benefits of both prostacyclin and stem cell therapies. The efficacy of this new therapy was tested in mice with hindlimb ischemia, an animal model of PAD. When injected into the ischemic muscle, the engineered hMSCs improved blood flow, enhanced muscle function, and promoted muscle regeneration better than the non-manipulated hMSCs did. The study results also indicated that the prostacyclin-secreting hMSCs protected resident cells from the harmful effects of ischemia and promoted the production of new cells by stimulating the body’s own repair mechanisms.
“This study shows that our novel approach of using hMSCs engineered to over-express prostacyclin provided benefits that were superior to those seen with non-engineered hMSCs,” says Richard A.F. Dixon, PhD, Director of the Molecular Cardiology Research Lab. “We believe these findings establish a paradigm for using manipulated stem cells to boost the body’s natural regenerative processes. This strategy could be used not only to improve therapies for PAD but also to develop more effective treatments for other cardiovascular diseases.”
The authors of the Nature Communications article are Yuxiao Deng, Zhongwei Yang, Toya Terry, Su Pan, Darren G. Woodside, Jingxiong Wang, Kehe Ruan, James T. Willerson, Richard A.F. Dixon, and Qi Liu.
###
About the Texas Heart Institute
The Texas Heart Institute, founded by world-renowned cardiovascular surgeon Dr. Denton A. Cooley in 1962, is a nonprofit organization dedicated to reducing the devastating toll of cardiovascular disease through innovative and progressive programs in research, education and improved patient care. Together with its clinical partner, CHI St. Luke’s Health – Baylor St. Luke’s Medical Center, it has been ranked among the top cardiovascular centers in the United States by U.S. News & World Report’s annual guide to “America’s Best Hospitals” for the past 24 years.
For media inquiries please contact:
Linden Emerson
713-850-2110

.svg)


