
Dr. Robert Paisley is an accomplished physician, researcher, and entrepreneur with extensive experience in cardiac electrophysiology and general cardiology.
Show full bioDr. Paisley graduated from Texas A&M University with a Bachelor of Arts in Biology and a minor in History, where he was recognized for his academic achievements by being inducted into Phi Beta Kappa, a prestigious national academic honors society.
He completed his fellowship in cardiovascular disease and subspecialty fellowship in cardiac electrophysiology at The Texas Heart Institute and Baylor College of Medicine after earning his Doctor of Medicine degree from the University of Texas Medical School at Houston and internal medicine training at Walter Reed Army Medical Center and Baylor College of Medicine.
Following medical school, Dr. Paisley began his military career as a commissioned officer in the U.S. Army Medical Corps. He completed an internship in internal medicine at Walter Reed Army Medical Center in Washington D.C. and volunteered for a combat deployment as the Battalion Surgeon for 3-509th Infantry (Airborne) at Joint Base Elmendorf-Richardson, Alaska.
Dr. Paisley’s awards and decorations include the Bronze Star for meritorious service while deployed to Afghanistan, the Army Commendation Medal, the Combat Medical Badge, the Parachutist Badge and the Royal Thai Army Parachutist Badge.
Dr. Paisley is committed to using his expertise in cardiac electrophysiology and cardiology to improve the lives of his patients and contribute to ongoing research in the field. His military background has taught him to be resilient and adaptable, qualities that he brings with him to his medical practice.
Texas Heart Institute Positions
- Cardiology & Electrophysiology, The Texas Heart Institute Center for Cardiovascular Care
Education
-
Undergraduate:
Texas A&M University
-
Medical School:
University of Texas Health Science Center - Houston
-
Residency:
Baylor College of Medicine
-
Fellowships:
The Texas Heart Institute and Baylor College of Medicine, General Cardiology
The Texas Heart Institute and Baylor College of Medicine, Clinical Cardiac Electrophysiology Fellowship
Publications
Recent News
Cardiac Electrophysiologist Dr. Robert Paisley Joins The Texas Heart Institute Center for Cardiovascular Care
HOUSTON (June 17, 2023) — The Texas Heart Institute Center for Cardiovascular Care is pleased to welcome Robert D. Paisley, MD,...
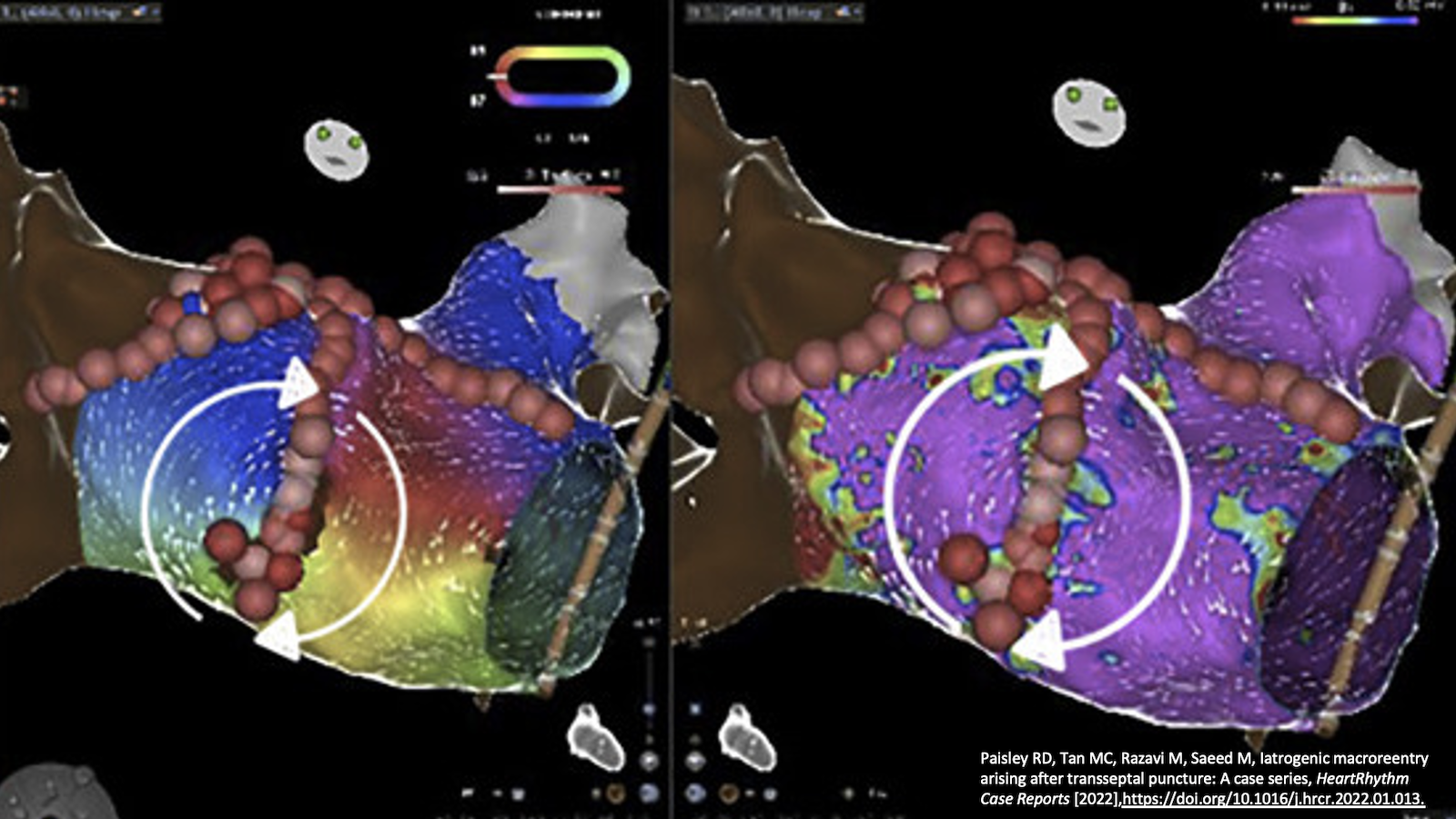
THI Doctors First to Describe an Uncommon Cause for Atypical Flutter
THI’s Clinical Cardiac Electrophysiology Research Team Discovers a Pattern of Macroreentrant Atrial Flutter Arising in Patients Who Underwent Transseptal Puncture...

A Remarkable Match — THI Welcomes New Cardiology Fellows
The THI Cardiology Fellowship program continues to recruit some of the best applicants in the nation. We had an outstanding...


