
Home > Texas Heart Institute at Baylor College of Medicine Awarded NIH Grant to Explore Immune Cell Role in Heart Failure
The Texas Heart Institute at Baylor College of Medicine’s Gene Editing Lab has been awarded a highly competitive NIH R01 grant from the National Heart, Lung, and Blood Institute (NHLBI). The prestigious award will fund groundbreaking research into how changes in the heart’s immune system contribute to the progression of heart failure.
Heart failure remains a leading cause of death and disability worldwide, affecting more than six million Americans. While current treatments help many patients, they cannot fully prevent the heart’s gradual decline. To address this challenge, researchers are turning their attention to a previously overlooked factor: specialized immune cells in the heart known as macrophages.
At the forefront of this effort is Dr. Xiao Li, Assistant Professor and Principal Investigator of the project. Dr. Li’s laboratory has led pioneering studies demonstrating how diseased macrophages drive the progression of heart failure. The newly awarded NIH R01 grant recognizes his innovative work and will provide critical support to advance his research on developing immune-based therapies for heart failure.
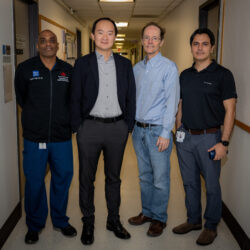 Working alongside Dr. Li is a distinguished team of co-investigators from the Center and Texas Children’s Hospital, including Dr. James Martin, Dr. Arash Pezhouman, and Dr. Diwakar Turaga, whose combined expertise spans molecular medicine, cardiovascular biology, and critical care medicine. The project further benefits from collaborators at Northwestern University, including world-leading immunologist Dr. Edward Thorp, establishing a strong, multidisciplinary partnership.
Working alongside Dr. Li is a distinguished team of co-investigators from the Center and Texas Children’s Hospital, including Dr. James Martin, Dr. Arash Pezhouman, and Dr. Diwakar Turaga, whose combined expertise spans molecular medicine, cardiovascular biology, and critical care medicine. The project further benefits from collaborators at Northwestern University, including world-leading immunologist Dr. Edward Thorp, establishing a strong, multidisciplinary partnership.
“In a healthy heart, macrophages play a protective role by keeping tissues balanced and clearing away damage,” said Dr. Li. “But in heart failure, we’ve discovered these cells can become senescent, or aged, and instead of helping, they begin releasing harmful signals that worsen heart injury.”
The project will explore three critical questions:
Using cutting-edge tools, including single-cell genomics, computational biology, patient-derived heart tissue models and animal models, the team aims to uncover the mechanisms that drive immune cell “aging” in the failing heart. These insights could open the door to entirely new therapies that target macrophage senescence, slowing or even halting heart failure progression.
“This project has the potential to transform how we think about treating heart failure,” Dr. Li added. “If we can find ways to reverse these harmful immune changes, we may be able to offer patients a future with healthier, stronger hearts.”
The work is an important step forward in the Center’s mission to push the boundaries of cardiovascular science and improve outcomes for patients worldwide.
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/

Visit U.S. News & World Report