Dr. Cohn is an active member of the Professional Staff at THI and served as Director of the Center for Technology and Innovation and Director of the legendary Cullen Cardiovascular Research Laboratory at the THI prior to joining Johnson & Johnson, as the Vice President for Medical Devices Companies and Executive Director of the new Center for Device Innovation at the Texas Medical Center in Houston.
Show full bioDr. Cohn earned an undergraduate degree in Biology and Chemistry from Oberlin College in Ohio, and went on to receive his Doctor of Medicine from the Baylor College of Medicine in Houston, Texas. He then completed seven years of general surgical and cardiothoracic surgical training at the Baylor College of Medicine Affiliated Hospitals and a one-year cardiothoracic fellowship at Boston’s Beth Israel Hospital. After completion of his training, he stayed on as a staff Cardiothoracic surgeon at the Beth Israel Deaconess Medical Center and as a full-time faculty of Harvard Medical School for ten years before being recruited back to his hometown.
At THI he has been intimately involved in the development of the continuous-flow, totally implantable, artificial heart and in 2011, Dr. Cohn and Dr. O. H. Frazier successfully implanted the first pulseless total heart replacement device in a human patient.
Medical device development remains his passion and he has been granted more than 90 US patents or patents pending for his medical innovations that have provided the core technology for six venture-backed medical start-ups.
His numerous awards include an honorary doctorate in science from Oberlin College, the Distinguished Scientist Award, given by the MacDonald Fund, and the Edison Award for excellence in human-centered design and innovation for the SentreHEART® Lariat®. In 2000, Dr. Cohn was named the distinguished Inventor of the Year by the U.S. Intellectual Property Owners Association. In 2014 he was named Outstanding Inventor of the Year by the Houston IPO. In addition, in 2014 he received the Innovation award at ICI in Tel Aviv for inventing the TVA everLINQ system for percutaneous AV fistula creation and for founding TVA Medical. In 2015, he was awarded a Lifetime Achievement Award for healthcare innovation by the Houston Technology Center.
Before joining J&J, he was a Venture Partner at Santé Ventures and was the Chief Medical Officer for BiVACOR USA and for Reliant Heart.
Texas Heart Institute Positions
- Teaching Staff, Cardiac Transplantation, Heart Failure and Assist Device Fellowships
- Teaching Staff, Thoracic Surgery Residency
Education
-
Undergraduate:
Oberlin College
-
Medical School:
Baylor College of Medicine
-
Internship:
Baylor College of Medicine
-
Residency:
Baylor College of Medicine
Academic & Clinical Affiliations
Honors, Awards and Memberships
Publications
Recent News
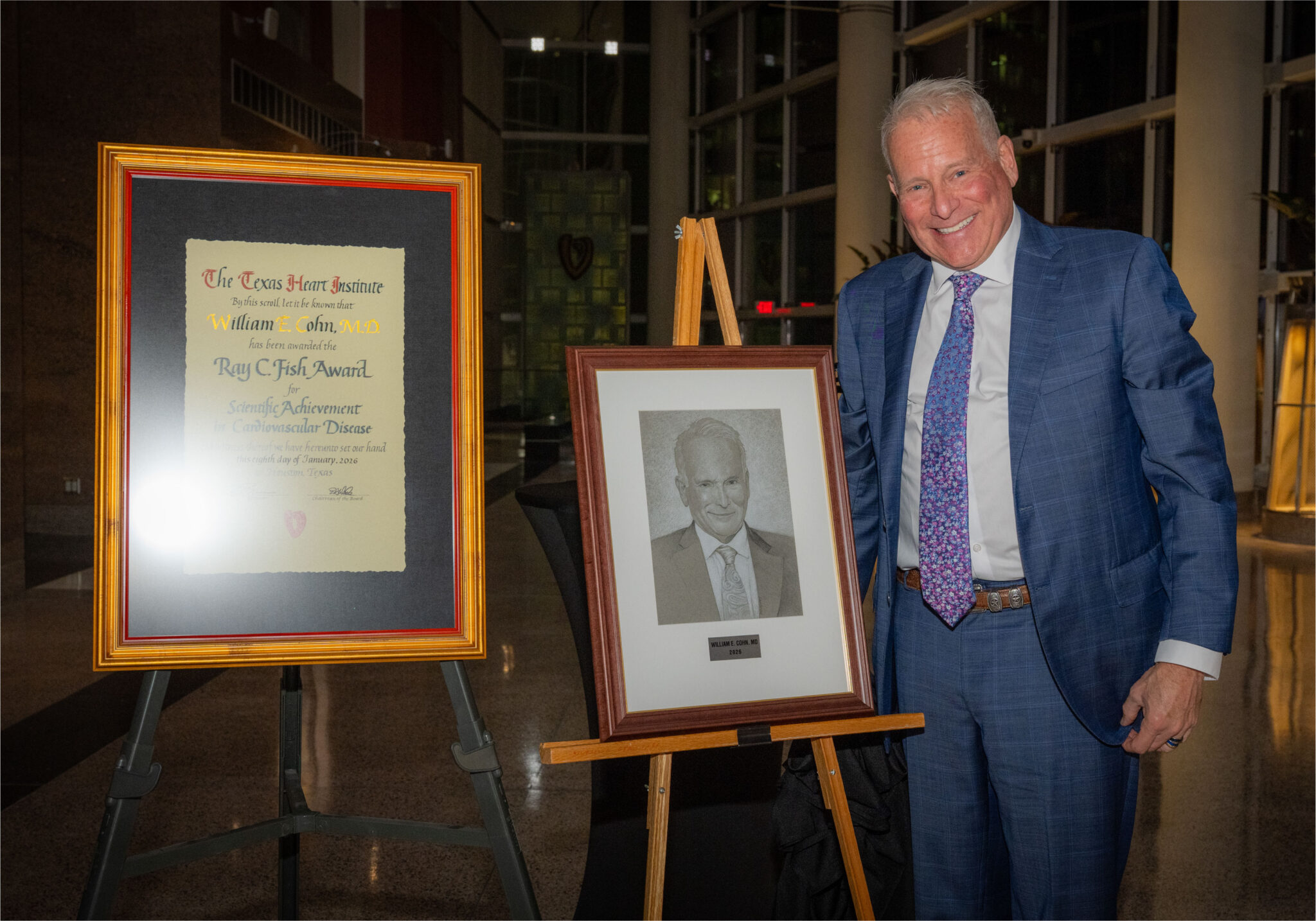
A Legacy of Invention: Dr. Billy Cohn and the Spirit of Innovation at The Texas Heart Institute
Some careers follow established paths. Others create entirely new ones. For decades, William E. Cohn, MD, known to colleagues and...

The Texas Heart Institute Hosts 2024 Rodeo Roundtable: Cardiogenic Shock
On Saturday, March 2, 2024, The Texas Heart Institute hosted THI Rodeo Roundtable 2024: Cardiogenic Shock, a discussion group chaired...

THI Continues to Play a Pivotal Role in the Latest Development in the Field of Artificial Heart Technology
The Texas Heart Institute partner, BiVACOR, gets additional support Total Artificial Heart program With plans for an FDA-granted investigational...


