
Home > Electrophysiology Team Pioneers Safer, Smarter Approach to Treating Dangerous Heart Rhythms as Published in Nature
Published in Nature Biomedical Engineering, the breakthrough highlights a novel energy-based technique that could transform the future of arrhythmia care worldwide.
Researchers at The Texas Heart Institute at Baylor College of Medicine’s (THI) Electrophysiology Clinical Research & Innovations Lab, led by Dr. Mehdi Razavi, along with students and researchers at the Department of Electrical and Computer Engineering, Rice University, have published a landmark study in Nature Biomedical Engineering that could transform the future of cardiac care. The paper, Distributed battery-free bioelectronic implants with improved network power transfer efficiency via magnetoelectrics, details a new system of wireless, battery-free implants designed to deliver precise electrical stimulation within the body.
 The THI team includes Kavya Sinha, Mathews John, Drew Bernard, Lukas Jaworski, and Payam Safavi-Naeini, who have worked alongside collaborators at Rice University, and Houston Methodists, to demonstrate the clinical potential of this novel technology.
The THI team includes Kavya Sinha, Mathews John, Drew Bernard, Lukas Jaworski, and Payam Safavi-Naeini, who have worked alongside collaborators at Rice University, and Houston Methodists, to demonstrate the clinical potential of this novel technology.
The team addressed a longstanding challenge in cardiac electrophysiology. Current implantable devices such as pacemakers and defibrillators rely on wires (leads) threaded through blood vessels into the heart. While lifesaving, these leads can limit how many pacing sites physicians can use, restrict optimal placement, and increase the risk of complications.
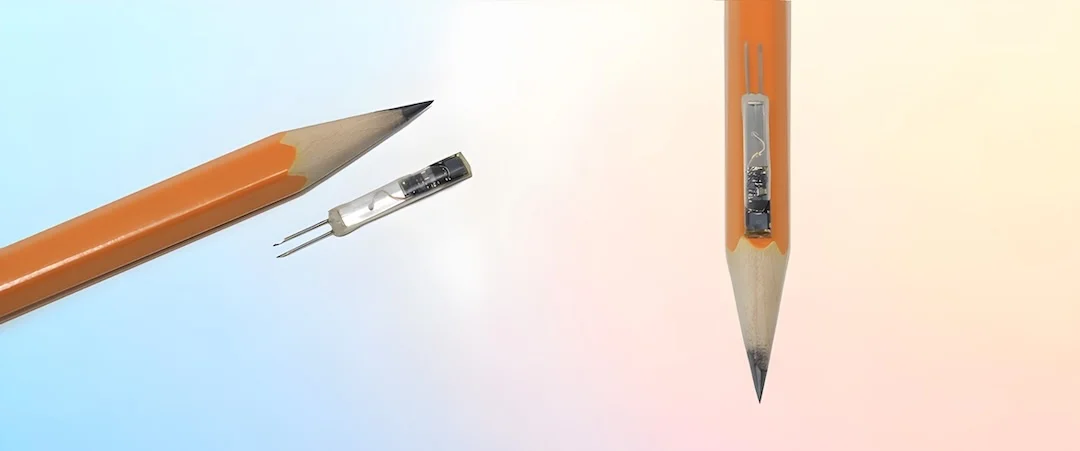
Pacing device detail with a pencil for scale. (Image courtesy of Joshua Woods)
The study introduces a new approach: miniature, battery-free implants powered wirelessly through magnetoelectric materials. These materials convert magnetic fields into usable electricity, allowing multiple implants—each about the size of a grain of rice—to be powered and controlled by a single external transmitter. Remarkably, the system becomes more efficient as more implants are added, enabling coordinated stimulation across multiple points in the heart.
The THI team successfully tested three wireless pacemaker nodes on the surface of a pig’s heart, showing they could coordinate activity to modify and stabilize heartbeat rhythms. The THI team includes Kavya Sinha, Mathews John, Drew Bernard, Lukas Jaworski, and Payam Safavi-Naeini, who have worked alongside collaborators at Rice University, and Houston Methodists, to demonstrate the clinical potential of this novel technology.
This proof-of-concept directly addresses limitations in cardiac resynchronization therapy (CRT), a treatment for heart failure. CRT is currently constrained by how many leads can be safely placed in the heart. By contrast, the wireless approach offers:

The system exploits the properties of magnetoelectric materials, which convert magnetic fields into electricity using mechanical vibrations. (Photo by Gustavo Raskosky/Rice University)
“This technology paves the way for remarkably innovative and highly impactful advances in the field of cardiac electrophysiology, the most important of which is enabling painless, imperceptible cardiac defibrillation,” said Dr. Razavi. “Defibrillator shocks, though lifesaving, can be traumatic for patients. By enabling the distribution of current across multiple pacing sites, this technology could vastly improve how patients experience these medical events.”
The success of this research marks a pivotal step toward next-generation cardiac therapies that are less invasive, more customizable, and ultimately safer for patients. With further refinement, these wireless pacing nodes could become a viable alternative to traditional pacemakers and resynchronization devices, reshaping how clinicians treat complex heart conditions.
At THI, the Electrophysiology Clinical Research & Innovations Lab continues to advance technologies that push the boundaries of what’s possible in cardiac care—always with the patient experience at the center of innovation.
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/

Visit U.S. News & World Report